A life application is received for $500,000 on an eight-month-old infant. The amount is reasonable in comparison to the parents. This is the first child in this family. The child’s birth and early physician checks were completely unremarkable except for the family’s refusal to vaccinate their child at all. APS states that although the pediatrician encouraged routine immunizations, the family is part of an active anti-vax community in their town. Neither mom nor dad have been vaccinated.
Is this child at increased mortality risk compared to others who are receiving their vaccinations as scheduled?
Principles of vaccination
The immune system’s job is to recognize “self” and tolerate that substance and also to recognize and eliminate “non-self” material. Protection from infectious diseases is highly reliant on this system.
The infectious organism, be it viral or bacterial, should be recognized as “non-self” and eliminated. Immunity may be acquired actively by producing antibodies by the organism’s own
cells or passively by obtaining antibodies from some other place, such as from the mother through the placental circulation or from injections as with Intravenous Immune Globulin (IVIG) infusions.
Although both are effective means of protection, active immunity tends to be longer lasting than passive immunity. Active immunity tends to last many years and is often lifelong. Passive antibodies degrade over time, and the individual’s own cells have no way of producing more antibodies. The initial presentation of the foreign particle or antigen stimulates a host of reactions resulting in antibody formation.
After a period of time, the level of antibodies may fall, but the reexposure of the immune system to the foreign substances reactivates the memory cells to very rapidly reestablish protection. Vaccinations work on this active immunity principle.
Community or herd immunity provides indirect protection from a pathogen. It describes resistance of circulation of a disease due to a sufficient number in the community with immunity to that particular disease. This offers protection to those not immune, such as newborns, the chronically ill or the unvaccinated, from encountering the disease because those who are immunized do not spread the disease.
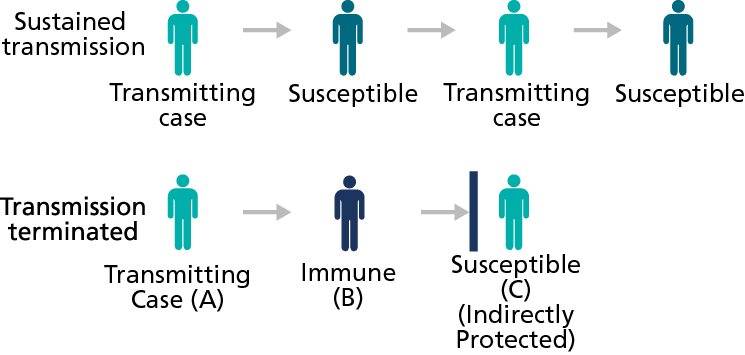
Figure 1 - Herd immunity
The percentage required to be immune to prevent disease varies by infectious agent. Measles and rubella outbreaks have occurred in communities with 85-90% immunization levels. The principle holds that as immunization levels drop below a certain threshold, the non-immune will no longer benefit from the indirect protection.
Vaccine hesitancy or refusal
In the United States, all states have laws requiring some immunizations for school entry. However, all states allow medical exemptions, and most allow religious or philosophical
exemptions. The American Academy of Pediatrics’ website has an interactive map listing the percent of children immunized by vaccine type and state as well as whether or not the state allows nonmedical exemption. The range of nonmedical exemptions varied by state in 2016-2017, from <0.1 – 7.5%. Parental objections to vaccination also vary.
Nonmedical parental objections to vaccine:
- Concern for vaccine safety, perceived or real
- Lack of efficacy
- Belief that natural illness is better
- Fear of overwhelming an infant’s immune system
- Unaware of seriousness of an illness
- Lack of trust in authority figures (medical, public health, pharmaceutical companies)
- Religious or moral objectives
2019 child & adolescent immunization schedule
The recommended child and adolescent immunization schedule for 2019 has been approved and promoted by the CDC, the American Academy of Family Physicians and the American Academy of Pediatrics. Canadian recommendations are similar, though not exactly the same, and they vary by province.
In general, the first immunization is received in the hospital after delivery, Hep B #1, and then the shots are obtained at roughly two, four and six months of age, followed by doses between
12-18 months with boosters given at around five years before school attendance. There is a little variation in the 12-18 month range, particularly if there are local “epidemics” of a specific
illness. Some of the ranges noted in the chart have to do with the specific formulations of vaccines that are available at the time of vaccination. These schedules have been studied extensively. The timing of the inoculations is such to optimize the child’s immunologic response while trying to have protection in place at the age when disease spread is most prevalent and/or most dangerous to an individual.
Some childhood vaccinations are recommended to protect patients from chronic illness or cancers in their adult years, such as Hepatitis B (HepB) vaccine and Human Papilloma Virus (HPV) vaccine. They are in place in childhood because some viruses that are found to cause cancers in later adulthood are actually acquired asymptomatically at very young ages. Because of these facts, variations to the schedule are not encouraged. There is a separate “catch up” schedule which can be found on the CDC’s website for those who were not vaccinated on schedule. Again, timing of the vaccines is very important for an optimal immunologic response.
Protecting individuals and groups
Some vaccinations are put in place to protect the individual from an illness that can vary from mild to severe but, more importantly, to protect a susceptible group from serious illness. This would include pertussis, in which mortality is disproportionately borne by the very young who cannot mount an immune response, and rubella, which is most devastating to pregnant women and their unborn fetuses. Congenital Rubella Syndrome (CRS) was a major cause of fetal loss and neonatal morbidity with life-long implications in the pre-vaccine era.
Vaccines and screening programs are put in place as a response to current threats and concerns. They must be economical and beneficial. There must be a benefit to morbidity, mortality and/or financial loss to remain efficacious. Tetanus, diphtheria, measles, mumps, polio, hepatitis A, influenza, rotavirus, Hemophilus influenza B and pneumococcal disease all fit into this category. These diseases are still present throughout the world, even though they may be greatly contained in developed countries with high immunization rates. As such, travel, immigration and waning immunity from low vaccination rates are all that are needed to
reintroduce these pathogens or accelerate their transmission in previously well controlled regions.
As with treatments, one must balance the risk versus benefits. How much is too much? Can a young child respond immunologically to the vaccine? Do the short-term costs (in money and time) outweigh the long-term benefits (lack of acute illnesses or future cancers)?
Several vaccines have been developed and successfully implemented with positive results only to find that immuneprotective properties wane over time. That is how some recommendations have changed from single vaccines or initial series to a series that is followed by a booster several years later. Most are familiar with tetanus shots. In general, a tetanus shot is recommended every 10 years in an otherwise healthy individual, but if five years have passed since the last immunization and a patient presents with a serious or potentially soil-contaminated
wound, a tetanus booster shot is given.
Similarly, measles, mumps, varicella and pertussis vaccines, while initially recommended as only a single vaccine or a short series, now all have the recommendation of future booster injections. Time has proven that immunization wanes, and protection is much less complete than hoped for at times distant from initial inoculation.
These charts obtained from the Centers for Disease Control and Prevention website demonstrate both the reduction in incidence of vaccine responsive illness and the effect on mortality.
Returning to the case
In this case, there appear to be both favorable and unfavorable signs. On the positive side, the family sees the pediatrician regularly and likely seeks care when needed. On the negative side,
the parents are unvaccinated and are part of a vibrant non-vax community, so the child is less likely to benefit from community or herd immunity.
Overall, given the levels of vaccination in the US and the incidence of vaccine preventable illnesses in the past few years, there is likely little to no increased mortality risk in this individual case. However, the overall vaccination situation needs to be monitored. With lower levels of vaccination in the community, one would expect increased risk in the vulnerable populations.
References
- www.cdc.gov/vaccines/pubs/pinkbook/index.html
- www.cdc.gov, last accessed 8/12/2019
- Fine, Paul, Ken Eames, and David L. Heymann. ““Herd immunity”: a rough guide.” Clinical infectious diseases 52.7 (2011): 911-916.
- Roush, Sandra W., Trudy V. Murphy, and Vaccine-Preventable Disease Table Working Group. “Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States.” Jama 298.18 (2007): 2155-2163.
- Public Health Agency of Canada, Vaccine Coverage in Canadian Children Results from the 2015 Childhood National Immunization Coverage Survey (cNICS), Ottawa, ON, Minister of Health, March 2018.