Currently in the United States, there are more people over the age of 20 years with CHD than under that age. The population of adult CHD patients is growing at a rate of 5% per year, with 1 to 1.3 million people in the U.S. and 2.3 million in Europe having ACHD. Estimates suggest that there are approximately 50 million ACHD patients worldwide, with a suspected steady increase in prevalence in 2050 projections.
While infant mortality due to congenital heart disease in the last four decades has decreased by almost three-fold, adult congenital heart disease prevalence has increased by more than two-fold in the United States. Over 85% of infants with CHD are now expected to reach adulthood. This is a result of the enhancement in diagnosis, including prenatal, refined surgical techniques and modern medical interventions such as the use of prostaglandin and infant cardiopulmonary bypass.
As would be expected, those patients with simple lesions, such as shunt defects atrial septal defects (ASD), ventricular septal defects (VSD) or patent ductus arteriosus (PDA), have a much lower mortality rate and therefore a higher prevalence in ACHD than those with severe lesions such as transposition of the great arteries or a single ventricle. Some of the mild noncyanotic lesions may not be diagnosed until adulthood.
Most common defects and causes of mortality
According to the Dutch CONgenital CORvitia (CONCOR) national registry for ACHD, the most common defects seen in adult patients are atrial septal defects, ventricular septal defects, tetralogy of Fallot, aortic stenosis, aortic coarctation, pulmonary stenosis, transposition of the great arteries, Marfan syndrome and bicuspid aortic valve.
Figure 1 - Proportional distribution of main diagnoses among 6,933 study subjects
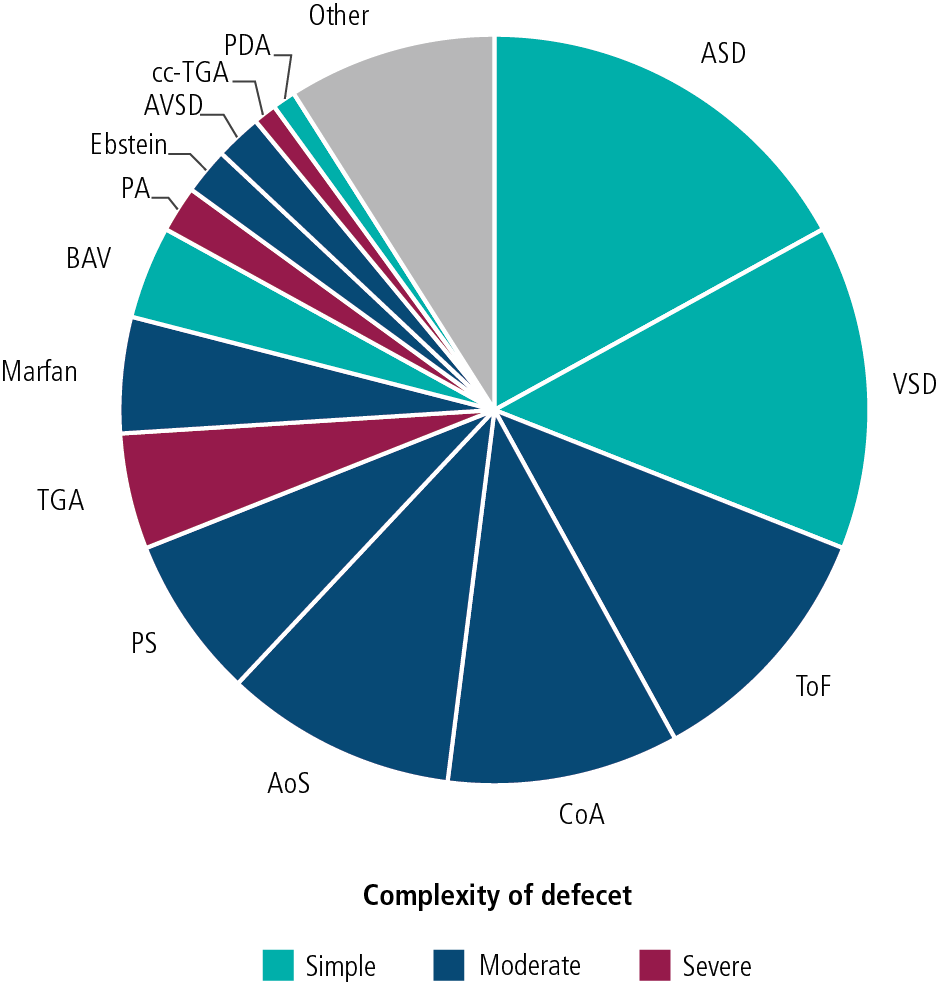
AoS – aortic stenosis (10%)
ASD – atrial septal defect (17%)
AVSD – atrioventricular septal defect (2%)
BAV – bicuspid aortic valve (4%)
CoA – aortic coarctation (10%)
Ebstein – Ebstein’s anomaly (2%)
Marfan – Marfan syndrome (5%)
Other – congenital heart defects with n, 65 (9%) | PA – pulmonary atresia (2%)
PDA – patent arterial duct (1%)
PS – pulmonary stenosis (7%)
TGA – transposition of great arteries (5%)
cc-TGA – congenitally corrected transposition of the great arteries (1%)
ToF – tetralogy of Fallot (11%)
VSD – ventricular septal defect (14%) |
Source: Verheugt, Carianne L., et al. “Mortality in adult congenital heart disease.” European Heart Journal 31.10 (2010): 1220-1229
Chronic heart failure (26%) and sudden death (19%) were the causes of death recorded most often. The median age at death from heart failure was 51.0 years (range: 20.3–91.2 years) and median age at sudden death was 39.1 years (range: 21.0–78.2 years). Two-thirds of patients died from a cardiac cause; 77% of deaths had cardiovascular origins, which would include all cardiac causes plus vascular causes such as pulmonary embolism and stroke.
Figure 2 - Proportional distribution of causes of death by defect in 197 deceased patients
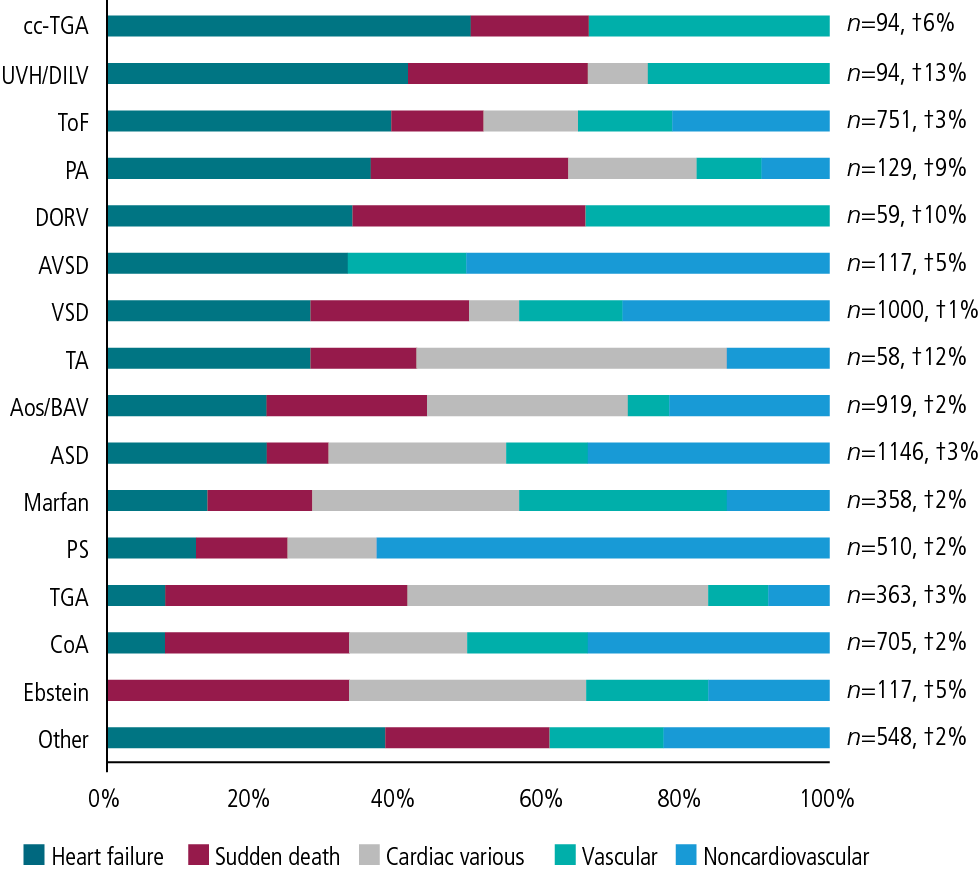
AoS – aortic stenosis
ASD – atrial septal defect
AVSD – atrioventricular septal defect;
BAV – bicuspid aortic valve
CoA – aortic coarctation
DORV – double outlet right ventricle
Ebstein – Ebstein’s anomaly
Marfan – Marfan syndrome
Other – less than three deaths [patent arterial duct, common arterial trunk, left ventricular outflow tract obstruction, mitral valvar prolapse, anomalous pulmonary venous connections, aortic regurgitation, aortopulmonary window, and atrial situs inversus | PA – pulmonary atresia associated with ventricular septal defect
PS – pulmonary stenosis
TA – tricuspid atresia
TGA – transposition of the great arteries
cc-TGA – congenitally corrected transposition of the great arteries
UVH/DILV – univentricular heart/double inlet left ventricle
ToF – tetralogy of Fallot
VSD – ventricular septal defect |
Source: Verheugt, Carianne L., et al. “Mortality in adult congenital heart disease.” European Heart Journal 31.10 (2010): 1220-1229
Sudden cardiac death (SCD) is of particular concern in ACHD patients. In the Concor study the seven defects with the greatest known risk of late SCD are univentricular heart, transposition of the great arteries, Ebstein’s anomaly, aortic coarctation, aortic stenosis, double outlet of right ventricle and pulmonary atresia.
Factors related to excess mortality
To examine factors related to excess mortality in a cohort of patients with ACHD, JM Oliver et. al. conducted a survival analysis in Spain using prospective data of 3,311 adults with CHD, with a median follow-up time of 10.5 years. Independent risk factors for excess mortality were identified by the left-truncated Cox regression model and include among others:
- cyanosis
- univentricular physiology
- genetic syndromes
- systemic ventricular dysfunction
- pulmonary hypertension
- pulmonary outflow tract obstruction
- infective endocarditis
Survival of individuals with no risk factors did not differ from the reference population. In contrast, the standardized mortality ratio (SMR) was 5.22 (95% CI 4.5–6.0; P< 0.001), and the median age at death for patients with at least one risk factor was 55.6 years.
Compared with age at diagnosis, sex and time of follow-up-adjusted expected survival for the Spanish general population, the SMR of 2.64 for the entire cohort was significantly higher (95% CI 2.3–3.0; P < 0.001) and increased progressively with the level of complexity of the defect. There was also an excess mortality for each underlying heart defect that ranged from 1.49 in patients with aortic valve disease to near 30-fold in patients with single ventricle physiology or pulmonary vascular disease.
Overall, adult survivors with CHD have globally reduced survival compared with the general population, with substantial variations relating to CHD complexity, repair status and specific CHD. Clinical parameters, such as anatomical features, hemodynamic sequelae or acquired complications, account for the early mortality of the contemporary ACHD population. Those who have required a repeat surgical procedure are also at greater risk for mortality. Importantly, survival of individuals with no risk factors did not differ from the reference population.
In terms of insurance medicine, the graph below summarizes the difficulty in estimating an excess of mortality in ACHD. Only by taking into account the complexity of the defect, the repair status and the risk factors can one come to an accurate and meaningful risk assessment.
Figure 3 - The difficulty in estimating excess mortality in ACHD
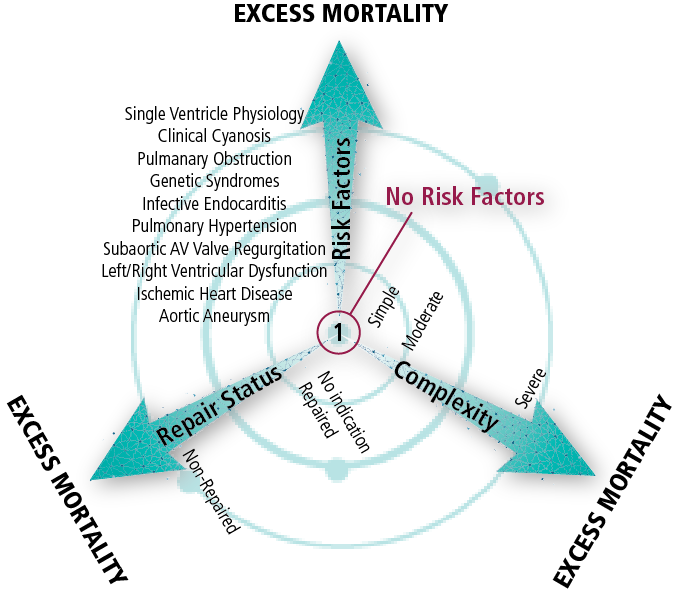
Source: Verheugt, Carianne L., et al. “Mortality in adult congenital heart disease.” European Heart Journal 31.10 (2010): 1220-1229
References
- Best, Katie E., and Judith Rankin. “Long-term survival of individuals born with congenital heart disease: a systematic review and meta-analysis.”
Journal of the American Heart Association 5.6 (2016): e002846.
- Oliver, Jose Maria, et al. “Risk factors for excess mortality in adults with congenital heart diseases.”
European Heart Journal 38.16 (2017): 1233-1241.
- van der Linde, Denise, et al. “Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis.”
Journal of the American College of Cardiology 58.21 (2011): 2241-2247.
- Verheugt, Carianne L., et al. “Mortality in adult congenital heart disease.”
European Heart Journal 31.10 (2010): 1220-1229.
- Warnes, Carole A. “Adult congenital heart disease: the challenges of a lifetime.”
European Heart Journal 38.26 (2016): 2041-2047.
-
Center for Disease Control: Heart Defects