A 34-year-old female is applying for $1 million of life insurance. Records reveal she was recently evaluated for a skin eruption mostly involving the distal extremities but which also involved the oral mucosa. There were minimal prodromal symptoms of mild fever and malaise present. There also was a history of an outbreak of herpes simplex approximately eight days prior to the onset of this skin eruption. She had been on no medications for the last several months.
The rash was described as having “target” lesions. An urgent evaluation was recommended as there was some concern by the provider initially evaluating the rash that this might be early Stevens-Johnson Syndrome (SJS). An ER visit occurred followed by a dermatological consultation. A clinical diagnosis of erythema multiforme was made. Topical corticosteroids were prescribed. Complete resolution of the symptoms occurred quickly and this was well documented during a follow up evaluation three weeks later.
What are the mortality considerations for someone with a diagnosis of erythema multiforme?
Erythema multiforme (EM) is a dermatological eruption which has been associated with a hypersensitivity reaction.
EM most commonly occurs in adults 20-40 years of age; however, it can occur in patients of any age. There are numerous conditions associated with this disease. Infections are believed to be the etiological agent in up to 90% of cases with herpes simplex virus (HSV) being the most common. Other infectious agents associated with EM include mycoplasma pneumoniae, adenovirus, cytomegalovirus and multiple fungal infections. Drugs and vaccines have also been associated with the condition. Non-steroidal anti-inflammatory drugs, sulfonamides, antibiotics and vaccines for hepatitis B and diphtheria-tetanus have all been implicated.
With HSV associated erythema multiforme the pathogenesis is felt to be a delayed-type hypersensitivity reaction. HSV-viral DNA fragments are transported by peripheral blood mononuclear cells to distant skin sites. CD4+ Helper T cells become involved and initiate an inflammatory response. This inflammatory response then appears as an erythematous rash.
The rash is frequently sharply demarcated and slightly raised from the surface of the skin. Its periphery is pink or red and the central portion develops a darker red, sometimes purpuric color (Figure 1). This appearance of the rash is referred to as a target lesion with 1 or 2 concentric zones surrounding this central darker area. However, the appearance of the rash frequently varies on the same patient, thus the term “multiforme”. The rash is typically distributed in a symmetrical fashion, frequently involving the extensor surfaces of the distal extremities but can be on the face, neck and/or trunk.
Oral mucous membrane lesions are common with EM, impacting patients in ~70% of the cases. Lesions may involve the lip, the buccal or labial mucosa or tongue.
When associated with herpes simplex the EM lesions typically appear two to 17 days after a herpes simplex outbreak, develop over a three-day period and resolve in approximately two weeks.
Figure 1 - Erythema Multiforme
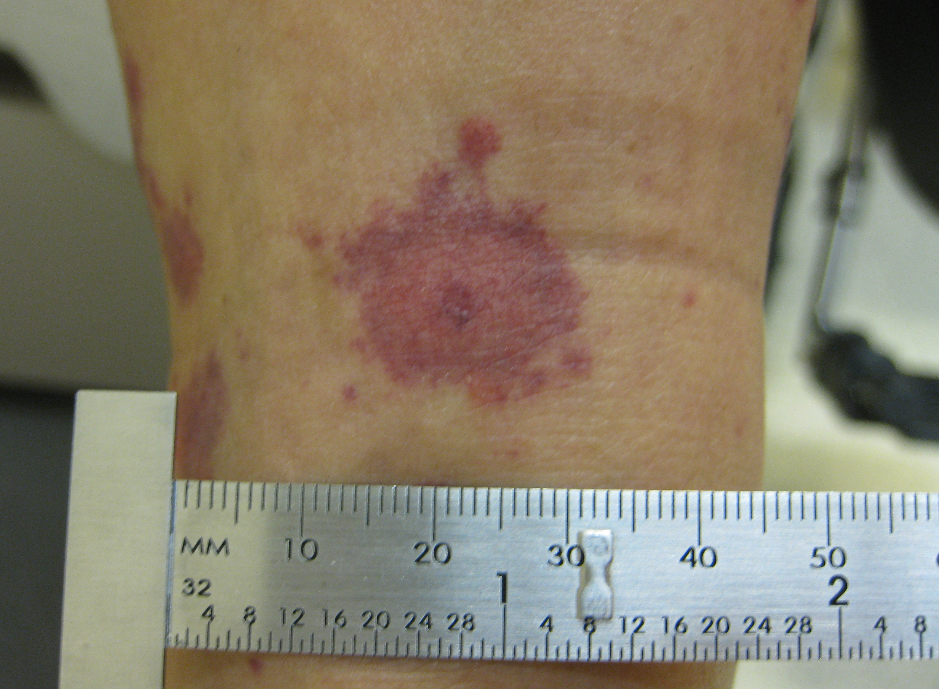
Accessed picture using Google’s “Labeled for reuse with modification” 8/7/2017.https://upload.wikimedia.org/wikipedia/en/d/d1/Target_lesion_1.jpg
EM is frequently an isolated event; however, it can be recurrent and at times can be persistent with lesions lasting several weeks or even months.
The diagnosis is most commonly made clinically by history and exam, but skin biopsies are occasionally necessary and can help exclude other conditions. Bullous pemphigoid and cutaneous small vessel vasculitis may present with a similar rash and require a biopsy and direct immunofluorescence studies for definitive diagnosis.
Stevens-Johnson Syndrome (SJS) has historically been confused with EM as well and, at one time, many believed these two diseases might be a variation of the same condition. However, currently these two dermatological eruptions are felt to be distinct. SJS is more commonly drug induced, and the rash is more macular compared to the papular nature of EM. SJS is typically a much more severe condition than EM.
Given the typical self-limited history of EM, treatment is generally symptomatic and limited to pain and pruritus interventions. However, for more severe cases, systemic glucocorticoid therapy may be required. Antiviral agents are frequently used when EM becomes recurrent.
Mortality is not typically adversely impacted with EM. However, it is important when confronted with a rash like this that the other causes of similar appearing rashes that have been associated with adverse mortality results (e.g., SJS, toxic epidermal necrosis, pemphigoid or paraneoplastic pemphigus) are eliminated from the differential diagnosis.
The overall mortality rate for Stevens-Johnson syndrome and toxic epidermal necrosis ranges from 5% to 19% in the US based upon a recent study. Bullous pemphigoid mortality is felt to range from 11%-48% based upon a variety of international studies. Rarely, EM can be associated with malignancy or confused with paraneoplastic pemphigus.
Returning to the case
In this particular case, the clinical diagnosis of erythema multiforme was made. No definitive biopsy was done but the history of a preceding HSV infection, the presence of the characteristic rash and the complete resolution of the symptoms is reassuring. It appears there is minimal to no excess mortality risk.
References
- Hsu, DY, et al. Morbidity and Mortality of Stevens-Johnson Syndrome and Toxic Epidrmal Necrolysis in United States Adults. J Invest Dermatol. 2016 Jul; 135(7): 1387-97
- Lee, JH, Kim SC Mortality of patients with bullous pemphigoid in Korea. J Am Acad Dermatology. 2014; 71 (4): 676
- Gual A, et al. Mortality of bullous pemphigoid in the first year after diagnosis: a retrospective study in a Sapnish medical centre. J Eur Acad Dermatol Venereol. 2014 Apr;28(4): 500-6
- Welter, D et al Pathogenesis, clinical features, and diagnosis of erythema multiforme. UpToDate. Topic updated Nov 15, 2016. Last accessed 8/8/2017.