A 49-year-old female is applying for life insurance. She was diagnosed with erythromelalgia three years ago. She experiences frequent episodes of severe pain and redness of her feet and hands. These episodes seem to be precipitated by mild changes in temperature or vigorous exercise.
Diagnostic testing included normal lower extremity doppler vascular studies. An electromyogram (EMG) was abnormal with the impression stating the criteria for axonal neuropathy were fulfilled. A complete blood count (CBC) done initially was normal. Repeat CBCs have been performed annually, and the most recent was abnormal with the WBC elevated at 18,000 per µL, platelets were slightly elevated, and the hemoglobin slightly reduced. A referral to a hematologist was made, but this evaluation hadn’t been completed at the time of the application.
There is a recent note mentioning the severity of the painful episodes has been mitigated satisfactorily with a combination of pharmacological use of gabapentin along with nonpharmacological use of icy water applied to the skin with onset of an exacerbation. The recent addition of daily aspirin has made a significant favorable impact.
What are the mortality considerations of a diagnosis of erythromelalgia?
Erythromelalgia is a rare disorder characterized by intermittent episodes of severe burning pain and marked erythema of the extremities. The condition was initially described in 1878 and named erythromelalgia, as it was very descriptive of the clinical findings.
The term was derived from the words: erythros (red), melos (extremity) and algos (pain). The disorder typically involves the lower extremities (most commonly the feet); however, it can occasionally also involve the upper extremities and/or the face
Precipitating factors for the intermittent symptomatic episodes include a mild increase in ambient heat or exercise. Unfortunately, there is no cure for the condition. There are however multiple treatment options, both pharmacological and nonpharmacological.
Treatment
These treatments have been successful in partial mitigation of the significant amount of pain and suffering that is associated with the condition. There is increased mortality from the condition centering mostly on the associated comorbid conditions, which includes myeloproliferative disorders. In addition, however, the symptoms of erythromelalgia can be so severe as to cause significant despair and depression leading to suicide.
Incidence
The incidence rate is one to two cases per 100,000 people per year. It is a condition which is more common in women. It is much more common in adults, but rarely children can be impacted.
The pathogenesis of the disorder is incompletely understood. The condition is most commonly sporadic; however, in approximately 6% of cases it is thought to be inherited. Most of the inherited cases impact children.
A gene located on chromosome 2q24 has been identified in the inherited cases. This gene produces a protein involved in a voltage-gated sodium channel which is important in normal nerve function. Thus far, at least 10 mutations have been identified, and hereditary erythromelalgia is inherited as an autosomal dominant condition.
When functioning properly, the voltage-gated sodium channels closely control the depolarizations in nerves including dorsal root ganglions and sympathetic ganglions. Abnormally functioning channels are associated with nociceptor hyperexcitability, which is associated with the pain in patients with erythromelalgia.
While erythromelalgia is most commonly seen as a stand-alone diagnosis, the disorder has been, at times, associated with a variety of other comorbid conditions. These comorbid conditions include myeloproliferative disorders (e.g., chronic myelogenous leukemia, polycythemia vera), pregnancy, drug exposures, neoplasms, autoimmune diseases and infections. Erythromelalgia is associated with an underlying myeloproliferative disease in approximately 8% - 10% of cases. Erythromelalgia can precede the myeloproliferative disorder, occur simultaneously or occasionally occur afterward.
Diagnosis
Typically the diagnosis of erythromelalgia is made through the characteristic clinical history and supported by abnormal findings on physical examination. Presenting symptoms include burning, numbness and increased heat.
Figure 1 — Examples of erythromelalgia

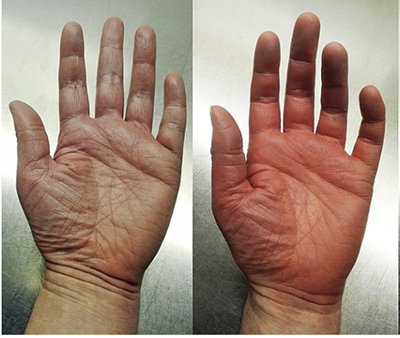
Feet image obtained 5/3/18 using Bing’s “Free to share and use commercially” search engine: https://jamanetwork.com/data/Journals/DERM/11693/dce9005f1.png
Hands image obtained 5/3/2018 using Google’s search engine “labeled for reuse with modification”: https://commons.wikimedia.org/wiki/
In one study1 feet were involved in 88% of cases, hands in 25.6%, legs in 13.7% and face in 3.5% of cases. Physical exam findings during an exacerbation include both a raised skin temperature as well as significant erythema. Precipitating factors involved in exacerbations include exposure to increased ambient heat (52%)1 and exercise (28.6%)1. There are no pathognomonic diagnostic tests available.
However, there are abnormal tests frequently associated with the condition. EMG and nerve conduction studies are frequently abnormal. Erythrocyte sedimentation rate testing is occasionally abnormally increased. Skin biopsies are frequently performed to eliminate other diseases which can present similarly, but the skin biopsy results in erythromelalgia, while abnormal, are typically variable and nonspecific.
Sometimes the diagnosis of this condition can be challenging given the intermittent nature of the symptoms. A cooperative partnership with the physician is sometimes needed so that a timely office visit evaluation occurs with the onset of the symptoms and signs.
Disorders in the differential diagnosis of erythromelalgia would include peripheral vascular disease, Raynaud phenomenon, cellulitis, acrocyanosis and various neuropathies.
Treatment
Treatment of erythromelalgia is directed at reducing the frequency and the severity of the symptoms. As is true for other conditions in medicine where there is no one consistently effective treatment available, multiple treatment modalities have been tried with varied success.
Avoiding precipitating factors is helpful. Nonpharmacologic treatment consists of intermittent fan use, limb elevation and timely application of cool water to the involved skin. Topical pharmacologic therapy includes anesthetics, capsaicin and gabapentin ointment. Systemic pharmacologic therapy includes aspirin (which is reported to be especially helpful in those with a comorbid myeloproliferative disease), gabapentin, amitriptyline, beta blockers and calcium antagonists among others. The multidisciplinary approach usually experienced at pain rehabilitation programs has been shown to be especially helpful.
Those with erythromelalgia are monitored frequently for response to treatment. Despair and depression are monitored closely and treated aggressively in those who don’t otherwise get good relief from the preventative and therapeutic maneuvers. Complete blood counts are regularly performed to monitor for the relatively rare, increased risk of myeloproliferative disorders.
Returning to the case
Erythromelalgia is associated with increased mortality risk. Most of the mortality risk centers around an increased risk for suicide in those who struggle obtaining adequate pain relief and the increased risk of comorbid conditions such as myeloproliferative disorders.
In this case documentation suggests the pain is under adequate control. However, the recent leukocytosis and thrombocytosis findings raise some concern about the possibility of a developing myeloproliferative disorder. It would be prudent to postpone until a full hematological evaluation has been completed.
References
Davis, Mark DP. et al Natural History of Erythromelalgia, Presentation and Outcome in 168 patients. Arch Dermatol. 2000; 136:330-336.
Davis, Mark DP et al. Erythromelalgia. UpToDate. Topic 13766 Version 3.0.
Accessed May 3, 2018.
Han, C. et al. Early-and late-onset inherited erythromelalgia: genotype-phenotype correlation. Brain, 2009. July;1711-1722.
Kalgaard, O.M. et al Erythromelalgia: a clinical study of 87 cases. Journal of Internal Medicine 1997; 242:191-197.
Mitchell, S. On a rare vaso-motor neurosis of the extremities, and on the maladies with which it may be confounded. Am J Med Sci 1878:76:17-36.